Reviewed by Cory J. Moczygemb, D.P.M | Podiatrist in San Antonio
That first step in the morning shouldn’t feel like walking on broken glass. Yet for millions of Americans suffering from plantar fasciitis, this stabbing heel pain is an unwelcome part of their daily routine. Whether you’re an active runner, a busy professional, or someone who spends long hours on your feet, understanding this common foot condition is the first step toward finding relief. At TSAOG Orthopaedics & Spine, our specialists are here to help!
Understanding Plantar Fasciitis
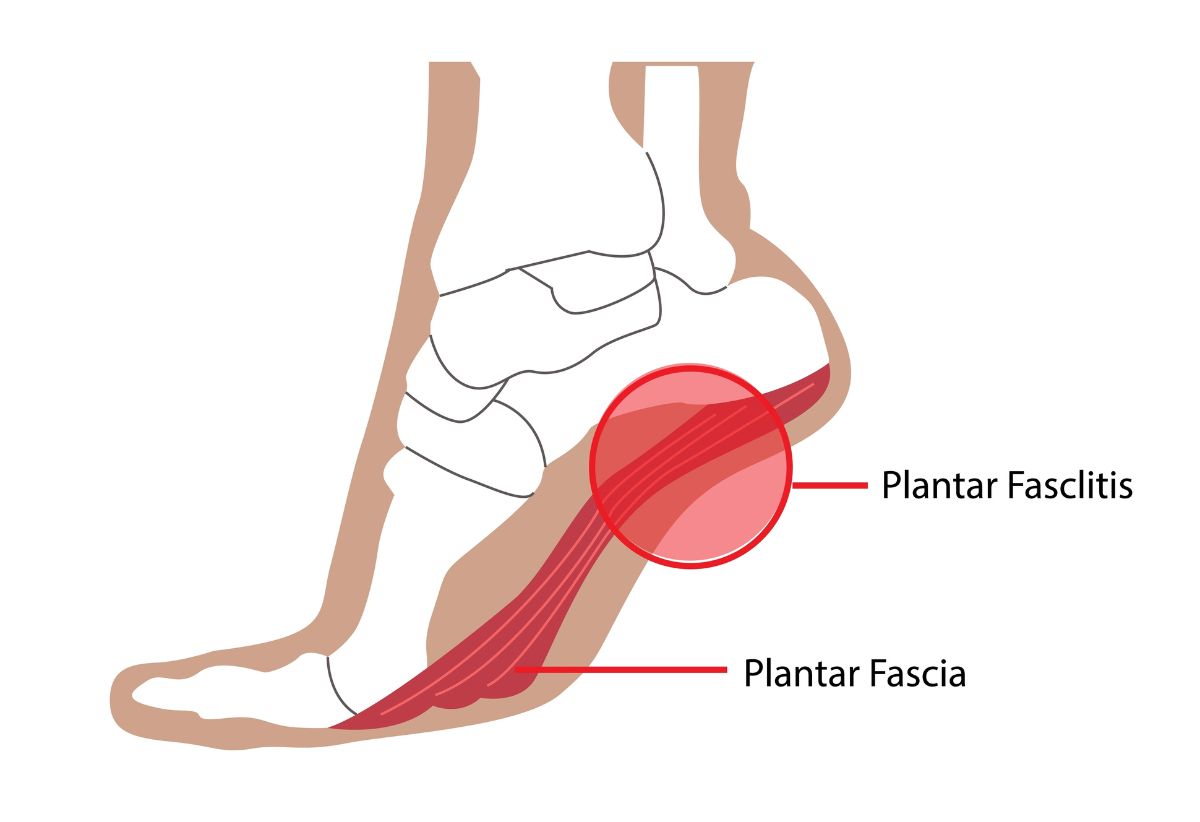
The plantar fascia is a thick, web-like ligament connecting your heel and the front of your foot. It functions as a shock absorber and supports the arch of your foot during weight-bearing activities.
Plantar fasciitis occurs when this ligament becomes inflamed, typically due to repetitive strain or excessive stress. This condition represents one of the most common causes of heel pain, affecting millions of Americans annually. The plantar fascia is designed to act like a bowstring, supporting the arch of the foot and absorbing the impact of walking, running, and jumping. If too much pressure damages or tears the tissues, inflammation and stiffness result. The condition typically develops gradually over time, though some cases may appear suddenly after intense activity.
Understanding the anatomy is crucial: the plantar fascia is not a muscle or tendon, but rather a thick band of connective tissue (fascia) that has limited blood supply, which can make healing a slower process. The condition can affect one or both feet and is particularly common in middle-aged individuals, though it can occur at any age. The structure of the plantar fascia is unique, consisting of three distinct segments – medial, central, and lateral components – with the central portion typically being the most affected in plantar fasciitis.
Plantar Fasciitis Symptoms
The hallmark symptom of plantar fasciitis is a sharp, stabbing pain in the heel, particularly noticeable with the first few steps in the morning or after prolonged periods of rest. This characteristic “first-step pain” occurs because the plantar fascia tightens overnight or during extended periods of inactivity. As you begin moving, the ligament gradually stretches, and the pain typically subsides, though it may return after long periods of standing or when rising from a seated position.
Many patients describe the sensation as feeling like they’re stepping on a knife or hot coal. The pain is usually localized to the heel area, specifically at the point where the plantar fascia attaches to the heel bone, though some people experience pain along the entire length of the fascia into the arch of the foot. Unlike some foot conditions, the pain often improves with initial activity but worsens as the day progresses, especially after prolonged weight-bearing activities.
Some people may also experience associated symptoms such as heel swelling, redness, or warmth. The pain pattern can be quite distinct: while it may temporarily improve with movement, extended periods of activity typically lead to increased discomfort, creating a challenging cycle for many sufferers who need to balance activity with rest.
Common Causes of Plantar Fasciitis
Plantar fasciitis develops from a combination of factors that put excessive stress on the plantar fascia.
- Biomechanics: One primary risk factor is biomechanical issues in foot structure, such as either very high arches or flat feet, which can affect weight distribution across the foot.
- Work: Occupational hazards play a significant role, particularly in professions that require long hours of standing or walking on hard surfaces, such as teachers, retail workers, and factory workers.
- Age: Age is another crucial factor, with the condition being most common between the ages of 40 and 60, as the plantar fascia loses some of its natural elasticity over time.
- Lifestyle Changes: Sudden lifestyle changes can also trigger the condition, such as beginning a new exercise routine, particularly high-impact activities like running or dancing, without gradual conditioning.
- Weight: Obesity or rapid weight gain significantly increases the risk, as extra weight puts additional stress on the plantar fascia.
- Pregnancy: Pregnant women often develop plantar fasciitis, especially in the late stages of pregnancy, due to both weight gain and hormonal changes that can affect ligament laxity.
- Footwear: Poor footwear choices, particularly shoes with inadequate arch support or worn-out soles, can contribute to the development of the condition by failing to properly distribute pressure across the foot.
How is Plantar Fasciitis diagnosed?
The diagnosis of plantar fasciitis typically begins with a comprehensive physical examination and detailed medical history. Healthcare providers usually start by asking about the pattern of pain, including when it’s most severe and what activities aggravate or relieve it.
During the physical examination, the doctor will touch and move the foot to identify specific areas of tenderness. The doctor may ask the patient to flex their foot to assess pain patterns and range of motion. They often perform specific tests, such as the windlass test, where the big toe is pulled back to see if it reproduces the pain.
While imaging tests aren’t always necessary for diagnosis, they may be ordered to rule out other conditions or confirm the diagnosis in unclear cases. X-rays might be taken to check for heel spurs or rule out stress fractures, while ultrasound can reveal the thickness of the plantar fascia and confirm inflammation. In some cases, MRI scans might be requested, particularly if standard treatments aren’t providing relief or if the doctor suspects another condition might be causing the symptoms.
The diagnostic process also typically includes a gait analysis to observe how the patient walks and distributes weight across their feet, as certain walking patterns can contribute to the condition.
Plantar Fasciitis Treatment Options
Like many other orthopedic issues, treatment for plantar fasciitis typically follows a progressive approach. Providers start with conservative methods before considering more intensive interventions. Each treatment option targets different aspects of the condition, from relieving immediate pain to addressing underlying biomechanical issues.
Stretching Exercises
Targeted stretching serves as the cornerstone of plantar fasciitis treatment. Key exercises include calf stretches against a wall, towel stretches performed first thing in the morning, and specific plantar fascia stretches that focus on lengthening the tissue. These stretches are most effective when performed multiple times throughout the day, particularly before taking the first steps in the morning and after prolonged periods of rest. The goal is to increase flexibility in both the plantar fascia and the Achilles tendon, which can help reduce stress on the heel.
Strength Training
Building intrinsic foot strength helps support the arch and reduce strain on the plantar fascia. Exercises such as toe curls, marble pickups, and arch raises target the small muscles of the foot that provide dynamic support during walking and standing. Additionally, strengthening the calf muscles through exercises like heel raises can improve overall foot mechanics and reduce stress on the plantar fascia. A physical therapist can prescribe conditioning exercises.
EPAT (Extracorporeal Pulse Activation Technology)
This non-invasive treatment uses pressure waves to stimulate blood flow and promote healing in the affected tissue. EPAT sessions typically last about 10 minutes and are performed weekly for several weeks. The treatment works by triggering the body’s natural healing response and can be particularly effective for chronic cases that haven’t responded to stretching and strengthening.
Surgery
Typically reserved for severe cases that haven’t responded to conservative treatments after 6-12 months, surgical intervention involves releasing part of the plantar fascia from its attachment to the heel bone (partial plantar fasciotomy). This is typically performed as a last resort due to the potential complications and extended recovery time. Surgery may be recommended when chronic heel pain significantly impacts daily activities and quality of life, but only after other treatment options have been exhausted.
Plantar Fasciitis FAQs
Should you walk with plantar fasciitis?
While complete rest isn’t usually necessary, it’s important to modify your activity level. Light walking can help maintain mobility, but avoid long distances or activities that cause significant pain. Listen to your body and take breaks when needed.
Can plantar fasciitis be healed?
Yes, plantar fasciitis can heal with proper treatment. Most cases improve within several months of consistent conservative treatment, though some chronic cases may take longer. The key is early intervention and following a comprehensive treatment plan.
What makes plantar fasciitis flare up?
Common triggers include sudden increases in activity, wearing unsupportive shoes, prolonged standing, weight gain, and changes in exercise routine. Additionally, skipping stretching routines or returning to high-impact activities too quickly can cause flare-ups.
Will plantar fasciitis go away by itself?
While plantar fasciitis might eventually improve on its own, without proper treatment, it can become chronic and take much longer to resolve. Active treatment typically leads to faster recovery and better outcomes.
What is commonly mistaken for plantar fasciitis?
Several conditions can mimic plantar fasciitis, including heel spurs, tarsal tunnel syndrome, stress fractures, and Achilles tendonitis. This is why proper medical diagnosis is important to ensure appropriate treatment.
Get Treatment for Plantar Fasciitis from TSAOG
Don’t let plantar fasciitis hold you back from living your best life. Since 1947, TSAOG Orthopaedics & Spine has been providing expert care to the San Antonio and South Texas community. Our team of over 42 orthopedic specialists, including dedicated foot and ankle specialists Dr. Kirk, Dr. Marx, and Dr. Robbins, along with our skilled podiatrists Dr. Moczygemba, Dr. Rustein, and Dr. Hughes, are here to help you find relief. Schedule an appointment today with one of our specialists and take the first step toward healing.