What is Osteoporosis?
Osteoporosis is a condition that causes your bones to become more brittle or soft and can lead to people having a higher risk of fractures. This is caused by losing too much bone as you age. The more bone you lose, the weaker the structure that holds them together. This in turn makes people that have been diagnosed with osteoporosis more susceptible to fractures, commonly from falls. In the United States, two million broken bones are caused by osteoporosis. So what should you be looking for before your bone health declines? We’ll go into that in the article below as we review the warning signs of osteoporosis and how it can be diagnosed and treated.
Early Warning Signs of Osteoporosis
Osteoporosis is often called a “silent” condition because there are very few symptoms that are noticed before the effects are felt. In most cases, people are diagnosed with osteoporosis when they sustain a fracture from a fall or injury. While symptoms may be hard to notice, there are certain factors that put people more at risk of developing osteoporosis.
These include:
- Women over the age of 50
- Men over the age of 70
- Vitamin D Deficiency
- Diabetes
- Rheumatoid Arthritis
- Certain Medications
- Family History of Osteoporosis
Unfortunately, you cannot feel your bones getting weaker overtime. So it is important to always be cognizant of yourself or people you may know who fall into these categories above. Fractures caused by osteoporosis can happen anywhere in your body. The most common places where people sustain these fractures are in hips and wrists.
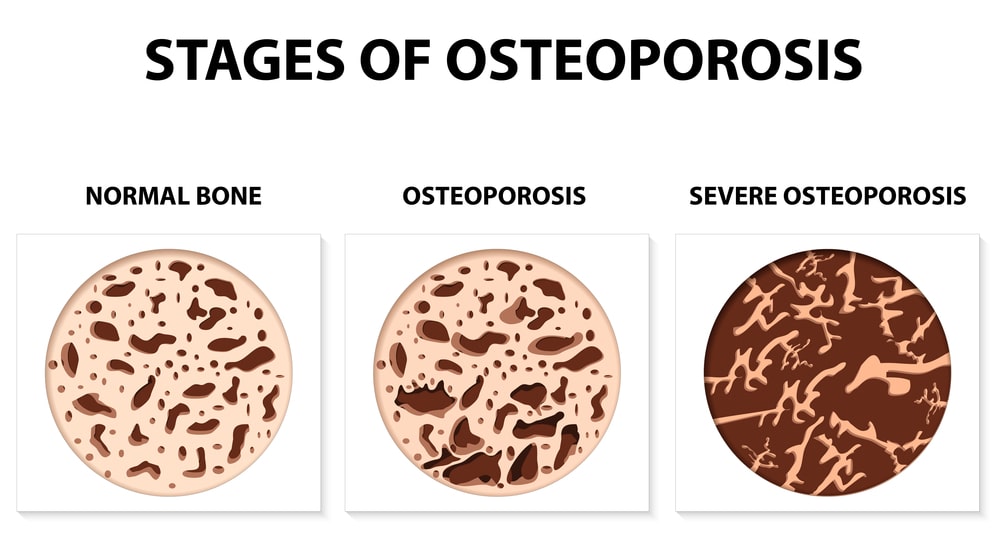
What Are the Stages of Osteoporosis?
Your body continuously adds bone as it loses it as you age. It is normal for you to make more bone than you lose while you are younger because you are growing. Around the age of thirty, this begins to slow down to the point where you stop increasing your bone density. There are multiple stages that lead to osteoporosis. Rather than occur from one day to the next, the gradual loss of bone determines which stage you might be in.
Stage 1: Normal Bone
At this point, your body has stopped adding to your bone density meaning that you no longer overproduce bone. This is fairly common for individuals around the age of 30.
Stage 2: Osteopenia
Osteopenia occurs when your body does not create new bone as fast as it can replace bone loss. Some causes can include a low-calcium diet, a history of smoking, age, or even certain medications.
Stage 3: Osteoporosis
If the effects of osteopenia continue, then you may reach the point of osteoporosis. This is due to the loss in bone density.
Stage 4: Severe Osteoporosis
This is the point at which people are most susceptible to fractures. People at this point have chronic pain issues or have limited mobility due to a low bone density.
Is it Possible for Osteoporosis to be Reversed?
As seen in the stages above, osteoporosis only gets worse the longer it goes undiagnosed. One question that a lot of patients have is can this condition be reversed? Unfortunately, you cannot reverse the bone loss that is caused from osteoporosis. That is why it is crucial that we diagnose this condition as early as possible in order to prevent further damage. So if learning that you have osteoporosis is so important, how do you diagnose if someone has it?
How is Osteoporosis Diagnosed/ Who can Diagnose It?
Typically, patients older than 60 who have sustained a fracture are recommended to receive a bone health evaluation. This is because it is likely that one of the reasons for the fracture can be linked to the effects of osteoporosis at that age. Bone health evaluations are a consultation visit where your healthcare provider reviews your history of fractures, history of falls, any medications you may be taking, and your current lifestyle habits. This information helps provide them with recommendation options on either treatment plans or possibly even further examinations.
History of Fractures & Falls:
Fractures that are obtained very easily or from short falls all point to signs of osteoporosis. While it is most common to experience these fractures from falls, any stress that is applied to the bones and causes a fracture should be noted.
List of Medications:
Certain medications may cause bone density to decrease which is called secondary osteoporosis. It is important to communicate with your healthcare provider any medications you have been prescribed.
Lifestyle Habits:
Your diet has an effect on the progression of bone loss as you age. It is important to eat foods that are high in vitamin D to help build stronger bone. Other factors such as exercise can help to prevent the progression of osteoporosis.
Bone health evaluations can be done by primary care doctors or orthopedic specialists. If a fracture is the initial reason for a visit, an orthopedic specialist can not only help aid in surgical repair of the injury, but also the osteoporosis treatment as well. At TSAOG, we have our bone health clinic where it is their mission to diagnose and treat patients with osteoporosis. If you feel like you could benefit from a bone health evaluation, make sure to schedule an appointment with our Nurse Practitioner for Bone Health, Janean Vargas today!
If your healthcare provider sees signs of osteoporosis after your bone health evaluation, further testing may be done such as a bone density test. A bone density test is designed to measure the content and overall strength of your bones.
Osteoporosis Treatment Options
As mentioned previously in the article, there is no way to reverse the effects of osteoporosis. However, your healthcare provider’s goal at this point is to preserve as much bone as possible. One of the ways they can do this is through providing various treatment options. These can include adjusting a patient’s diet, implementing a physical therapy plan, or even the use of medications in severe cases.
Diet & Supplements:
Calcium and vitamin D are essential in the production of bone. Meals that contain dairy and vegetables (high in calcium) or eggs and fish (high in vitamin D) are recommended to improve overall bone health. In some cases, the use of supplements can also be used to help aid in this process.
Physical Therapy:
Some of the exercises that patients can expect to complete to help with osteoporosis include weight-bearing exercises, balance training, and resistance training. These exercises help to put positive stress on your bones while also reducing the risk of fracture in the future.
Medications:
There are medications that can be prescribed to slow down the loss of bone. This method of treatment works with others to help aid in the bone-building process. While the medication helps to slow down this process, it is important to continue other forms of treatment that help promote your bone health to ensure the best results.
No matter what level of evaluation you receive from your healthcare provider, the goal of treatment is always to reduce the risk of fractures through increasing your bone density. While the effects of osteoporosis are not reversible, it is still possible to preserve your bone health before it gets worse.
FAQ’s about Osteoporosis
Can osteoporosis be cured?
Unfortunately, no osteoporosis cannot be cured. However, treatment options are put into place in order to manage the effects that osteoporosis has.
What not to do if you have osteoporosis?
If you get diagnosed with osteoporosis, you should avoid physical activities or exercises that put you at a high risk of falling. Weaker bones make you more susceptible to fractures so avoid putting unnecessary stress on your bones to avoid injury.
Do you feel tired with osteoporosis?
Some people with osteoporosis experience fatigue. While this does not mean that fatigue is a symptom, it could be a result of a lack of vitamin D which causes poor bone health.
How should you sleep with osteoporosis?
Sleeping on your back helps if you have osteoporosis because it distributes weight evenly across your body and maintains the alignment of your spine and hips.
What are bad foods for osteoporosis?
High-sodium foods, red meat, caffeine, and alcohol are all things you should avoid if you get diagnosed with osteoporosis. These foods and drinks reduce essentials like calcium and vitamin D, which are a main component in building bone.
Should I get a bone health evaluation if I have arthritis?
Yes you should get a bone health evaluation. Arthritis is a risk factor for osteoporosis and should be assessed with your healthcare provider.
If you feel you would benefit from getting a bone health evaluation or would like to learn more about your bone health, make sure to schedule an appointment with our Bone Health Clinic today using the link below.