Persistent ankle pain and stiffness can greatly affect your quality of life, turning everyday tasks like walking or climbing stairs into difficult challenges. When non-surgical treatments such as medication or physical therapy no longer provide relief, ankle replacement surgery may offer a lasting solution. This innovative procedure may help alleviate discomfort and restore mobility, enabling patients to return to the activities they love. Let’s explore the key aspects of ankle replacement surgery, from preparation to recovery, so you can make an informed decision about your care.
What Is Ankle Replacement Surgery?
Ankle replacement surgery, or total ankle arthroplasty (TAA), is a surgical procedure designed to replace a damaged ankle joint with an artificial implant. The ankle joint, also known as the tibiotalar joint, is where the shin bone (tibia) connects to one of the foot bones (talus). Arthritis often can impact this joint along with other joints in the foot. Over time, the smooth cartilage covering the surface of these bones can wear down, leading to pain, inflammation, and swelling in the affected joint. This procedure aims to mimic the natural motion of the ankle joint while significantly reducing discomfort caused by arthritis.
Who Needs Ankle Replacement Surgery?
Ankle replacement surgery is often recommended for individuals with severe arthritis of the ankle joint. Several different types of arthritis, each with distinct causes and characteristics, may lead to the need for this procedure.
Osteoarthritis
Osteoarthritis, often called “wear-and-tear arthritis,” is the most common form of arthritis affecting the ankle joint. It occurs when the protective cartilage that cushions the ends of the bones gradually wears away. As the cartilage deteriorates, bones begin to rub against each other, causing pain, stiffness, and swelling. Osteoarthritis is typically associated with aging but can also result from previous injuries or repetitive stress on the ankle. When the pain and limited mobility from osteoarthritis impact daily life and non-surgical treatments no longer help, ankle replacement surgery may be a viable option.
Post-Traumatic Arthritis
Post-traumatic arthritis develops after an injury to the ankle, such as a fracture, ligament tear, or dislocation. Even after the initial injury heals, the joint may experience accelerated wear and tear due to changes in its alignment or stability. Over time, this can lead to symptoms similar to osteoarthritis, including pain, swelling, and reduced range of motion. Post-traumatic arthritis often affects younger, more active individuals who sustained ankle injuries earlier in life. For those with severe post-traumatic arthritis, ankle replacement surgery may provide significant relief and restore mobility.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an autoimmune condition in which the body’s immune system mistakenly attacks the lining of the joints, causing chronic inflammation. In the ankle, this inflammation can damage cartilage, bones, and soft tissues over time, leading to pain, stiffness, and deformity. Rheumatoid arthritis often affects both ankles and can severely limit walking and other activities. Patients with advanced RA who have not responded to medications or other therapies may benefit from ankle replacement surgery to relieve pain and improve joint function.
Preparing for Ankle Replacement Surgery
A successful outcome begins long before you enter the operating room. Proper preparation sets the stage for a smoother surgical experience and a more efficient recovery process. Taking proactive steps ensures you’re physically and mentally ready for the procedure while minimizing potential risks and complications.
Have a Thorough Consultation
Schedule a consultation with an orthopedic specialist to discuss your specific condition and goals. During this visit, your doctor will explain the procedure, assess your suitability, and address any concerns. Your doctor should provide you with a list of preparation guidelines, including instructions on which medications to avoid before surgery and whether you can eat or drink on the day of the procedure. Open communication with your doctor is essential. Prepare a list of questions in advance, as your doctor will gladly address them to help you feel comfortable and fully prepared for the surgery.
Complete Preoperative Tests
Your doctor may request imaging studies, blood tests, and a physical examination to confirm you’re a good candidate for ankle replacement surgery. These assessments help identify underlying conditions that could affect the procedure or recovery.
Optimize Your Health
Improving your overall health before surgery can aid recovery. If you smoke, quitting before the operation is crucial, as smoking can impede healing. Maintaining a balanced diet, staying hydrated, and engaging in light exercise (if approved by your doctor) can also prepare your body for the physical demands of recovery.
Prepare Your Home for Recovery
Create a comfortable and accessible living space to support a smooth recovery. If possible, set up a temporary bedroom on the ground floor to eliminate the need for navigating stairs. Clear pathways of any obstacles to prevent tripping, and keep frequently used items within easy reach. To enhance safety, consider installing grab bars or railings in the bathroom and other high-use areas.
Arrange for Support
During the initial recovery period, your mobility will be limited, making it essential to have a reliable support system. Family, friends, or professional caregivers can help with everyday tasks such as cooking, cleaning, and grocery shopping, reducing stress as you heal. Additionally, make sure to arrange for transportation home following your surgery, as you won’t be able to drive yourself.
What to Expect During Ankle Replacement Surgery
Knowing what to expect before, during, and after the procedure can help you feel more confident and prepared for the experience. The surgery itself typically takes about 60 to 90 minutes to complete. Here’s a detailed look at what happens during the procedure to help you approach it with peace of mind.
Anesthesia
Before the procedure, you’ll receive anesthesia to ensure comfort. This could be general anesthesia, which puts you to sleep, or regional anesthesia, which numbs the lower half of your body.
Incision and Joint Access
The surgeon makes an incision to access the joint, usually at the front of the ankle. Damaged cartilage and bone are carefully removed to create a smooth surface for the prosthetic components.
Prosthetic Placement
The artificial joint consists of metal components for the tibia and talus and a plastic spacer that facilitates smooth movement. These parts are secured to the bone and aligned to mimic the natural joint motion.
Closing the Incision
Once the prosthetic joint is in place, the surgeon meticulously closes the layers of skin and muscle. The ankle is then immobilized in a splint to protect it during the initial healing phase.
What to Expect After Ankle Replacement Surgery
Recovery from ankle replacement surgery is a critical phase that requires patience, dedication, and a commitment to carefully following your surgeon’s instructions. This period is essential for ensuring the procedure’s success and restoring your ankle’s function and mobility. While the timeline and specific recovery steps may vary depending on your individual case, understanding what to expect can help you mentally prepare for the journey ahead.
Hospital Stay
You’ll likely remain in the hospital for 1–2 days so your medical team can monitor your recovery. Pain and swelling are common during this time, and your care team will provide medications to help manage these symptoms. Before you’re discharged, you’ll receive detailed recovery guidelines to follow at home, ensuring a safe and effective healing process.
Restricted Mobility
For the first week or so, it’s recommended to rest and elevate your leg. Weight-bearing is usually prohibited for a few months to allow the ankle to heal. You’ll need crutches, a walker, or a wheelchair to move around.
Physical Therapy
Rehabilitation begins early to restore strength, flexibility, and range of motion. Your physical therapist will guide you through exercises that promote healing and mobility.
Long-Term Recovery
It may take 6–12 months for full recovery. During this time, avoid high-impact activities and follow your doctor’s instructions carefully. Regular follow-up appointments will confirm the prosthetic joint is functioning properly.
Is Ankle Replacement the Best Option for You?
Deciding between ankle replacement and other treatments depends on your unique condition and goals. Ankle replacement is ideal for those seeking pain relief while maintaining joint flexibility, but it isn’t right for everyone. Consulting with an orthopedic specialist will help you explore the options and choose the treatment that best meets your needs.
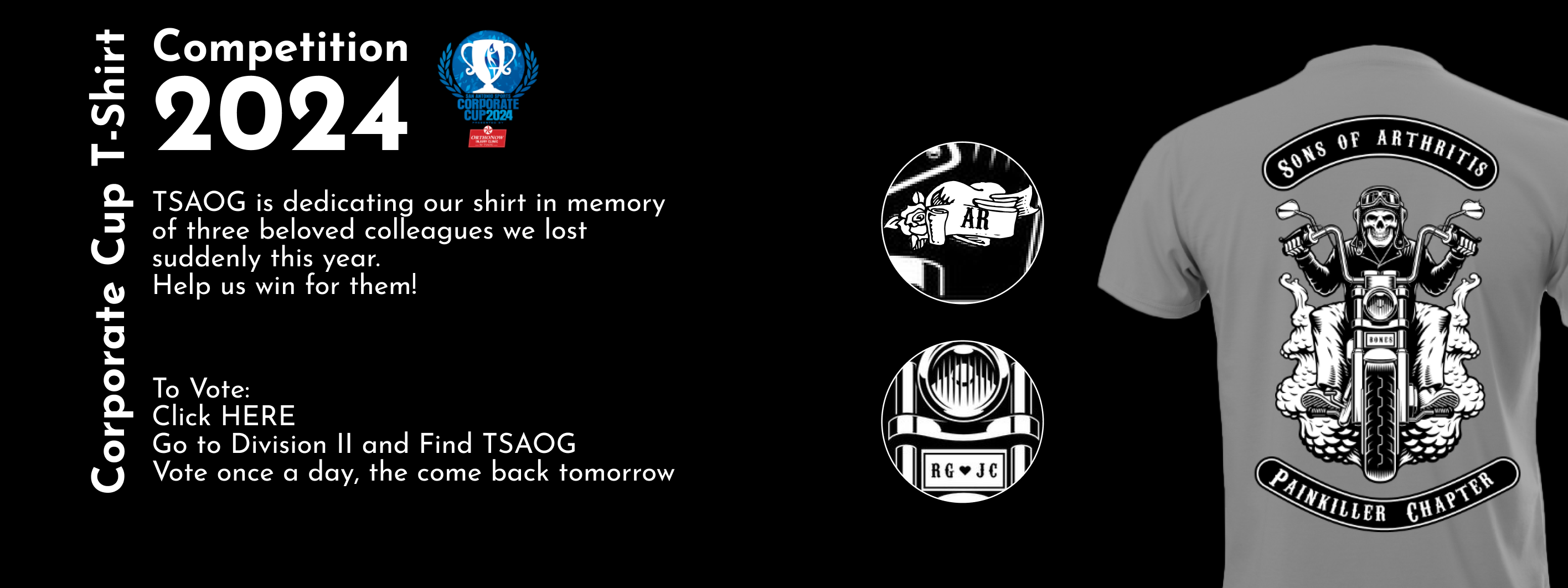
Trust TSAOG Orthopaedics & Spine for Expert Care
The orthopedic surgeons at the Foot & Ankle Institute of TSAOG Orthopaedics & Spine are board-certified and fellowship-trained in foot, ankle, and lower leg conditions. Their specialized training and extensive experience enable them to treat a broad spectrum of issues, ranging from common problems like bunions and hammertoes to complex reconstructions and total ankle replacements. Whether you need advanced surgical treatment or a non-surgical solution, our team is here to provide expert, patient-centered care.
Don’t let chronic ankle pain keep you from living the life you deserve. Schedule an appointment with one of our foot and ankle specialists at any of our convenient TSAOG Orthopaedics & Spine locations in San Antonio. Let us help you find the best solution for your ankle and get you back on your feet!